Antibiotics: Friend or Foe?
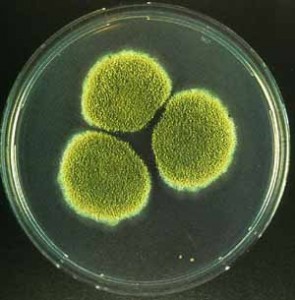 The trend is to abhor antibiotics. To decline their use no matter what, to tell your doctor that you will not allow such poisons into your system. But the truth is that antibiotics have been saving lives since the 1940's. Originally discovered by a French medical student, Ernest Duchesne in 1896, the first antibiotic, penicillin was not truly notable until its rediscovery by bacteriologist Alexander Fleming working in St. Mary's Hospital in London in 1928. He found that a plate culture of Staphylococcus had been contaminated by a blue-green mold and the colonies of bacteria adjacent to the mold were being dissolved. Currently this discovery has evolved into a billion-dollar business of more than 150 different antibiotics provided annually.
But because of the over-prescribing of antibiotics over the last thirty years, we have created super-bugs; bacteria that are resistant to just about any antibiotic treatment we can use. This makes infectious diseases disastrous, especially in close-quarter places such as hospitals and nursing homes.
The trend is to abhor antibiotics. To decline their use no matter what, to tell your doctor that you will not allow such poisons into your system. But the truth is that antibiotics have been saving lives since the 1940's. Originally discovered by a French medical student, Ernest Duchesne in 1896, the first antibiotic, penicillin was not truly notable until its rediscovery by bacteriologist Alexander Fleming working in St. Mary's Hospital in London in 1928. He found that a plate culture of Staphylococcus had been contaminated by a blue-green mold and the colonies of bacteria adjacent to the mold were being dissolved. Currently this discovery has evolved into a billion-dollar business of more than 150 different antibiotics provided annually.
But because of the over-prescribing of antibiotics over the last thirty years, we have created super-bugs; bacteria that are resistant to just about any antibiotic treatment we can use. This makes infectious diseases disastrous, especially in close-quarter places such as hospitals and nursing homes.
But originally, antibiotics were simple and amazing. Penicillin was first derived from mold, a fascinating explanation of the idea of homeopathy, since we can actually become incredibly sick from mold spores, yet mold is the very thing that can subdue a bacterial infection. In fact, the ancient Egyptians, the Chinese and even the Indians had all been using molds to treat infected wounds for centuries.
So let's take a moment to understand an antibiotic. It is by its very definition any chemical substance produced by one organism that is destructive to another. In other words, it is when life can be used to destroy another life. And we often forget that the majority of our illnesses are the result of two factors: an imbalance in the colonies of pathogens that live within our bodies all the time, and a simultaneous weakness in our immune and elimination systems that would normally control these colonies and mitigate any "infection" that would occur.
Antibiotics have a definite place in our world and in our health options. The trick is to know where that place is. Here are a few facts that will help you begin to define that place:
1) Antibiotics are only effective when used for a bacterial infection. Bacterial infections are generally localized to an area and can cause redness, swelling and especially pain. Viral infections are not responsive to antibiotics and are generally painless and involve entire body systems or more than one body area.
2) Antibiotics may only be effective when given at specific stages of illness. Every infection goes through stages, and often the initial infection can weaken the body, opening the door to "opportunistic" infections. So often there may be a bacterial infection, but concurrently a fungal or viral problem as well. So often antibiotics will only work on the bacterial issue, leaving the systemic problems untouched.
3) Antibiotics only act on bacteria that are replicating (not latent) which means that they are not as effective in chronic illness as they are in acute illness.
4) Antibiotics do not differentiate between our "good" necessary bacteria for health, such as our digestive bacteria, and the "bad" insidious bacteria. Most antibiotics are broad-spectrum and can create more disruption to our normal body ecology than the good they may do.
5) Antibiotics are provided in a "course". You must take the entire course in order to kill even the most resistant bacteria. If you fail to kill all the bacteria, then the ones that are most resistant can survive and mutate to resist that particular antibiotic.
6) Antibiotics are not completely metabolized in the body and can remain in the body systems long after the infection is resolved. They can also continue to be active even after excretion from the body, cascading into the environment. This is something to consider when you realize that more antibiotics are used on farmed animals than on humans. Therefore, the steak you eat may actually have active antibiotic strains still present.
7) Penicillin is the #1 cause of life-threatening anaphylactic shock. Be sure to read the information with an antibiotic to see what side effects are common, what interactions it may have and what the intended use is for a particular antibiotic.
So let's take a moment to look around at the place where you have ended up in this antibiotic journey. You have a specific infection in a specific area and it is recent (within 48 hours). If the infection is invasive, then you should consider taking an antibiotic, and it should be one that you have never taken before, or have not taken for at least a few years. That way the chances of the bacteria having any resistance are slim. So now that you have decided to take the antibiotic, here are some tips to making it as effective as possible:
1) Take the entire course (as mentioned above) to be sure to get even the most resistant bacteria on the first assault.
2) Many antibiotics can cause nausea, so try eating some toast or applesauce before taking your dose.
3) Get lots of rest so all your body resources can be directed to your immune system, taking advantage of the antibiotic presence.
4) Drink lots of green tea which actually increases the effectiveness of antibiotics.
5) Make sure to refrain from anything that interferes with the action of the antibiotic. Sometimes over the counter medication, certain minerals such as calcium or even alcohol consumption can all block the action of the antibiotic or increase the side effects.
6) Do not take probiotics during the time you are taking the antibiotic. It can actually detour the antibiotic's action. Instead, begin taking as soon as you complete your antibiotic course. If you are taking a long course of antibiotic therapy over several months, then you can take a probiotic at night before bed, away from your antibiotic dose.
Antibiotics are necessary, and useful. They save lives. But like all things, they have negatives as well. To get the most from taking an antibiotic, turn to them sparingly and take the entire course when you do, so that you don't have to do another round. They were developed to be life-saving and that is when they are at their best.
The trick to getting the most from an antibiotic is to prevent your body from becoming resistant. Following the guidelines listed here will help, but you can also turn to natural options when you need an antibiotic.
Try herbs with antibiotic qualities, such as Andrographis, Baical Skullcap, Baptisia, and Barberry. The strongest antibacterial agent in the herb world is Goldenseal, which is especially great for intestinal infections.
Cultures around the world know that many foods have wonderful antibiotic actions. The Chinese have used Reishi and Shiitake mushrooms for centuries, while the Indians of South America have turned to Cat's Claw which not only can handle bacteria, but concurrent viral and fungal infections as well. Lime juice has been used in India to reduce the infection of cholera, while garlic has been the basis of Italian immunity for centuries. Horseradish can protect against food-borne bacteria, while coconut oil can help to destroy pathogens by dissolving their protective layers. In fact, the active ingredient in coconut oil is lauric acid, which is also found in high concentrations in human breast milk.
My favorite recipe for bacterial infection is cinnamon and honey, a combination which is active against at least 60 strains of bacteria and has been effective for more than 2,000 years. Not that my grandmother was 2,000 years old, but she obviously knew a few things.
But getting back for a moment to the other factor in bacterial infection, your own immune strength and elimination health. The best defense is a good offense, so make sure that you support both with daily fiber ( I like Standard Process Whole Food Fiber), regular colonics to strengthen your muscular eliminative ability, and fill your diet with immune-strengthening foods. I recommend Standard Process Cataplex C tablets every day not only to strengthen the immune system, but to reduce C-Reactive protein levels. Then fill your plate daily with whole food vitamin C in strawberries, pineapples, kiwi, citrus fruits, cantaloupe watermelon, broccoli, cabbage, kale and cauliflower.
In this way, there will be fewer instances when you need medicinal antibiotics, and they will be so much more effective for you when you do. But you can also rest assured that advances in medicine and technology are being made knowing the problems with antibiotic use. Dr. Bonnie Bassler of Princeton University is following one promising path that is just an example of what we may see on the horizon. She is at the forefront of the growing field known as "quorum sensing" which is the study of how microbes, including bacteria, communicate with each other.
She has found that bacteria are not mindless. In fact, they are constantly through chemical signals, chatting about their numbers, their environment, and the dangers they face. It allows them to act as a group, like when more than 600 different species organize themselves into dental plaque or in bubonic plague when they can time their toxin release for maximum damage to the human host. This intricate web of communication among bacteria can even cross bacterial species creating multi-dimensional bacterial infections that are difficult to treat.
But exploring this communication language may have advantages. Rather than using an antibiotic that kills a bacteria outright, through quorum sensing, we can develop a therapeutic approach that would simply silence the molecular messages that induce bacteria to cause disease. An example of this is cystic fibrosis. In this congenital disease, mucous builds up in the lungs providing an environment for colonies of bacteria. These colonies in normal adults would be cleared up quickly by the immune system. But because of the chronic mucous, in cystic fibrosis patients, the infections never go away and one day the chronic illness becomes virulent and overwhelms the body causing death.
With a therapy based on blocking quorum sensing communication, the chemical messages that allow bacteria to act as a group would prevent the colonies from growing. Theoretically it could eliminate the fatality point of the disease and perhaps the disease itself.
Just remember that estimates show that there are 3000000000000000000000000000000 bacteria on the earth at any given time. So have some green tea...
